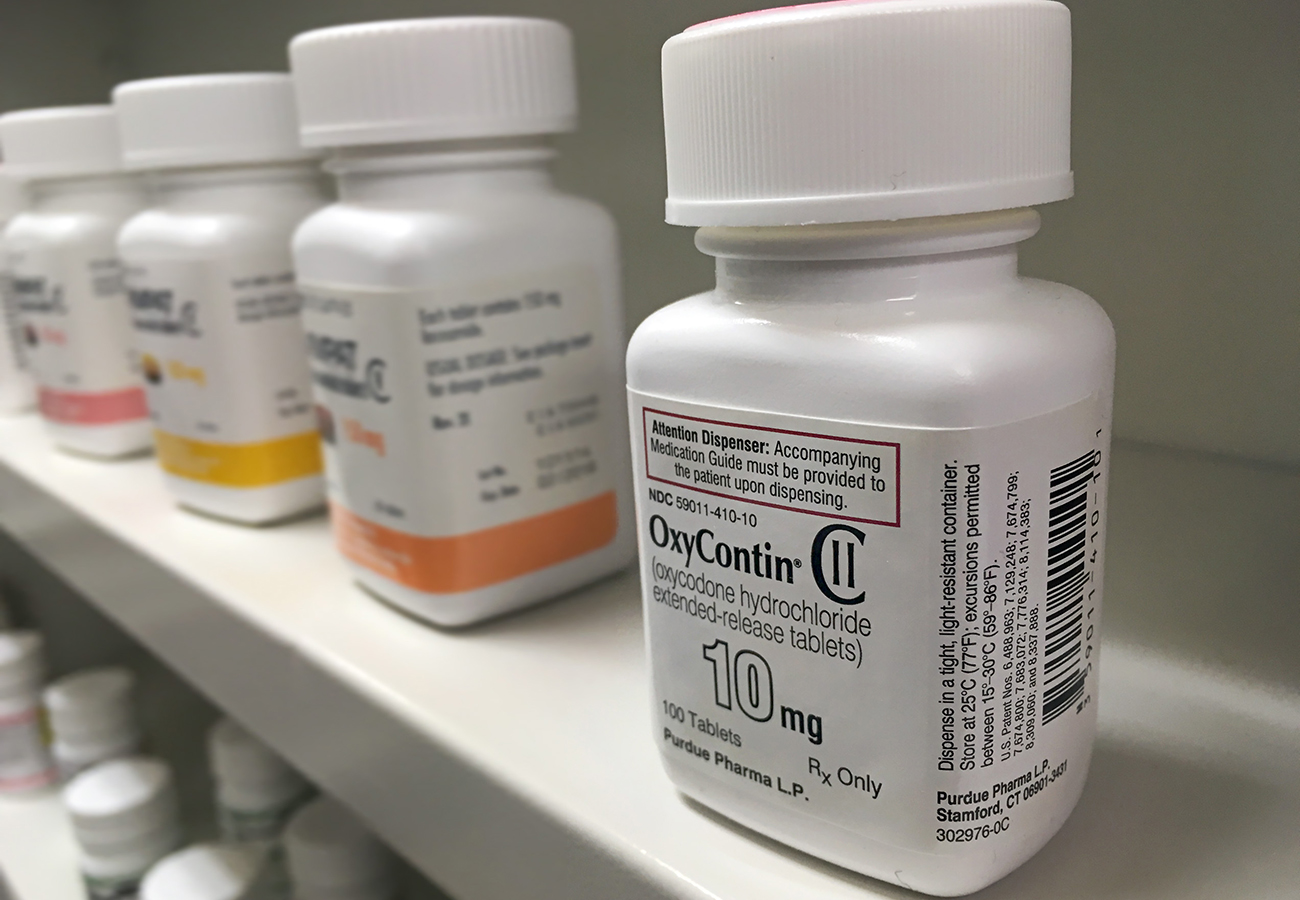
Prescription painkiller overdose is one of the leading causes of death in America right now, affecting millions of lives.
According to the Centers for Disease Control:
- In 2012, health care providers wrote 259 million prescriptions for opioid pain medication, enough for every adult in the United States to have a bottle of pills.
- Opioid prescriptions per capita increased 7.3% from 2007 to 2012, with opioid prescribing rates increasing more for family practice, general practice, and internal medicine compared with other specialties.
- From 1999 to 2014, more than 165,000 persons died from overdose related to opioid pain medication in the United States.
- In 2013, on the basis of DSM-IV diagnosis criteria, an estimated 1.9 million persons abused or were dependent on prescription opioid pain medication.
There is no question that prescription opioids are being abused by many who claim to have a pain disorder. These addicted individuals visit several doctors for the same conditions in order to obtain multiple prescriptions. They fake illness or injury to get drugs. They falsify prescriptions and buy painkillers from the black market. They manipulate the system in order to get the drugs they are addicted to. In fact, nearly 30% of patients prescribed opiates had no recorded pain diagnosis, according to the CDC.
Lives are being ruined and lost because of prescription opiates. In order to combat this epidemic, several laws and practices have recently been put into place. There are now stricter regulations for doctors who prescribe controlled substance, more comprehensive reporting required by pharmacists who fill the prescriptions, and more data collected on patients who are taking the medications. However, because of the increased security surrounding prescription painkillers, many who legitimately need pain medication for severe and chronic pain are sometimes unable to get the medications they need. The question remains, to what extent are we as a country willing to negatively impact pain patients in order to stop painkiller abusers and addicts?
CDC Recommendations For Opioid Prescription
The CDC published its guidelines for prescribing opioids in 2016, in an effort to help doctors, pharmacists, and even insurance companies aid in curbing unnecessary opioid prescribing and abuse and addiction. However, the CDC’s publication is simply a guide and is not mandatory, but because of some overzealous following of these suggestions, and fear of the growing opioid epidemic, some pain patients find it difficult and even impossible to get the pain relief they require. Below are some examples of the struggle pain patients face trying to get the medication they legitimately need to manage pain, according to a study published in Science Direct.
- Twenty-six states have passed laws that impose mandatory limits on the prescribing or dispensing of opioids for acute pain from surgery or an injury.
- Some pharmacies have placed restrictions on opioid prescriptions they will fill, limiting numbers of pills dispensed as well as denying prescriptions with dosages stronger than the CDC’s dosing guide.
- More than half of the pain patients surveyed (56 percent) reported disruptions in care or outright abandonment by their physicians.
- Some physicians are being red flagged for overprescribing, some even losing their licenses or facing criminal charges for overprescribing. Some physicians are now leery to prescribe at higher levels, even when necessary, in order to avoid scrutiny from the DEA or state medical boards.
- The state of Oregon is considering a proposal that would end coverage for opioids for many chronic pain patients on Medicaid. The original proposal would have forced pain patients to taper off their dose of painkillers in 12 months. Since its original consideration, last August, officials in Oregon have scaled back their proposal, to taper patients to 0 “when appropriate” based on the individual’s needs.
See the CDC guidelines here.
Pain Patient Statistics
According to the CDC report:
- The 1999–2002 National Health and Nutrition Examination Survey estimated that 14.6% of adults have current widespread or localized pain lasting at least 3 months.
- Based on a survey conducted during 2001–2003, the overall prevalence of common, predominantly musculoskeletal pain conditions (e.g., arthritis, rheumatism, chronic back or neck problems, and frequent severe headaches) was estimated at 43% among adults in the United States.
- Most recently, an analysis of data from the 2012 National Health Interview Study showed that 11.2% of adults report having daily pain.
- On the basis of data available from health systems, researchers estimate that 9.6–11.5 million adults, or approximately 3%–4% of the adult U.S. population, were prescribed long-term opioid therapy in 2005.
Reinterpreting The Guidelines
Some people wonder if the changes in prescription regulations are even helping. The rate of prescribing opioids has dropped every year since 2011, and still, opioid overdose deaths have continued to skyrocket during that same time frame.
Risks associated with denying prescription painkillers to pain patients include a loss of productivity, inability to function, medical decline, and increased risk of suicide. Individuals are losing their livelihoods and even their lives because they are unable to deal with chronic pain day after day.
The American Medical Association has recently pushed back against the misapplication of the CDC’s guidelines. At its meeting last November, the AMA adopted a series of resolutions describing its stance.
“Our AMA affirms that some patients with acute or chronic pain can benefit from taking opioids at greater dosages than recommended by the CDC Guidelines for Prescribing Opioids for chronic pain and that such care may be medically necessary and appropriate.
Our AMA advocates against the misapplication of the CDC Guidelines for Prescribing Opioids by pharmacists, health insurers, pharmacy benefit managers, legislatures, and governmental and private regulatory bodies in ways that prevent or limit access to opioid analgesia.
Our AMA advocates that no entity should use MME thresholds as anything more than guidance, and physicians should not be subject to professional discipline, loss of board certification, loss of clinical privileges, criminal prosecution, civil liability, or other penalties or practice limitations solely for prescribing opioids at a quantitative level above the MME thresholds found in the CDC Guidelines for Prescribing Opioids.”
Finding The Balance
So, what should be done? Prescription painkillers are addicting, and even when used as prescribed at first, can cause dependence and eventually addiction and drug-seeking behavior. First of all, we need to create better awareness of the dangers of any type of drug use. Doctors should try alternative forms of treatment whenever possible, and for those who require prescription opioids, they should be prescribed with care. Patients should be monitored closely for dependence and signs of abuse while on the medication, and patients should be screened for addiction prior to going on the medications.
On the other hand, physicians should be trusted enough to know which patients need more pain relief and should be allowed to prescribe based on the individual’s needs. Finding the balance between necessary pain relief and drug-seeking behavior is difficult, but if medical facilities take the CDC’s recommendations as just that and not requirements, we will provide more options for patients who desperately need this pain relief.
If you’re addicted to painkillers, you might need a detox program that can be monitored through residential or outpatient treatment facilities. Contact us now for more details.